Apr 8, 2020 | Native Hope
This April all communities around the world are striving to defeat an unseen killer among us—COVID-19. Coincidently, the U.S. Department of Health and Human Services Office of Minority Health [OMH] celebrates April as Minority Health Month, and the World Health Organization declares April 7 as World Health Day. Amid the COVID-19 outbreak, it is more important than ever to consider the effect such a pandemic has on minority communities, and the certain value our healthcare workers carry in protecting the underserved.

Social distancing in a tight-knit Native community where most homes are multi-generational and resources are slim is next to impossible. As Indian Country tries to prepare for the onslaught of COVID-19, many families live in fear of the unknown. Tribal Chairmen work to protect their nations with little support from the federal government. Congressional leaders like Deb Haaland, New Mexico Congresswoman, fight to ensure emergency funding reaches the tribes before the virus devastates reservations.
Indian Health Service clinics and hospitals [IHS], which provide healthcare for Native nations, are sorely underfunded. Like the states, the tribal nations rely on the federal government for emergency supplies during a national emergency. Currently, despite urgent requests from tribal leaders, funding for supplies and equipment for the COVID-19 crisis remains to be seen. Supplies are scarce. Yes, this sounds like the rest of the United States; however, the stakes are even higher for Native Americans.
The uphill battle through disparities
America’s Native population makes up less than 2 percent of the overall national population—around 6 million people. This population already faces extreme poverty. On many reservations 30-54% of the population falls below the national poverty line; whereas, the overall U.S. national poverty rate is 12.4%. To think it possible for the average family on a reservation in South Dakota to be able to feed the 8-12 people living in a home for 2 weeks is incomprehensible. Most families live week to week and some day to day.
Beyond the food insecurity problem, a large majority of Native Americans suffer from most of the health risks identified by the Center for Disease Control’s [CDC] risk factors for COVID-19. It has long been known that Natives have higher rates for diabetes, hypertension, heart disease, obesity, asthma, and several other life-threatening diseases. The health disparities between the average American and the Native American are profound.
 “’We’re already the poster child for the most vulnerable populations in this country,’” said Stacy Bohlen, the CEO of the National Indian Health Board, which represents tribal governments. “’This is not the place you want to skimp on resources if you want to hold the tide on this disease.’”
“’We’re already the poster child for the most vulnerable populations in this country,’” said Stacy Bohlen, the CEO of the National Indian Health Board, which represents tribal governments. “’This is not the place you want to skimp on resources if you want to hold the tide on this disease.’”
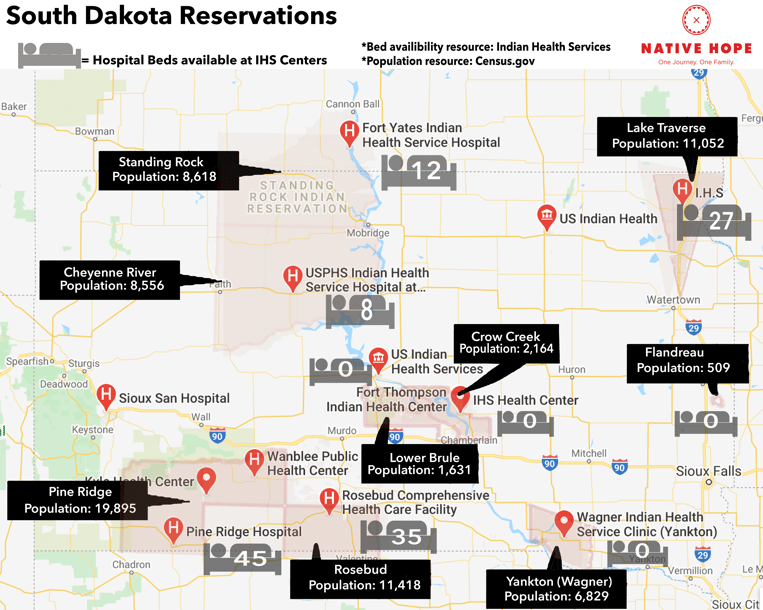
IHS facilities across the country have limited hospital beds and even fewer Intensive Care Units. “The Indian Health Service [IHS] does not have the medical providers, equipment, or facilities to treat critical patients. The IHS has 71 or fewer ventilators and 33 intensive care unit (ICU) beds at the 24 hospitals it runs.” It has also been reported by Health Affairs that “some frontline clinics received fewer than a dozen coronavirus tests, and federal officials have already signaled there will be little in the way of reinforcements — telling tribal leaders that all they can send right now are expired respirators.” In South Dakota, IHS facilities have fewer than 150 hospital beds to serve the over 70,000 citizens.
The effect on Native elders and children
Stacey Shields of the Crow Creek Sioux Tribe [Hunkpati Oyate] shares, “It’s terrifying to me. Everyday more and more of my hair is falling out because of the stress. Our IHS is not equipped…If someone gets infected, it will spread like wildfire. Practically every household here has a grandma, her kids, and her grandkids—all generations together.” She goes on to explain that even the hospitals within a half-an-hour are not equipped to handle COVID-19 and that for anyone in the area to seek adequate treatment, they will need to travel 3 hours to Sioux Falls, SD. Stacey has microscopic polyangiitis [MPA] a rare autoimmune disorder that causes bleeding in the lungs, kidneys, and other organs. As a result, she has had a kidney transplant and multiple other complications. “It I get this, I’m a goner.”
“We are preparing to go into battle with something we can’t see,” says Peter Lengkeek, a Hunkpati community member. He worries about the elders and the children. The elders hold the culture which is ever so valuable for the revitalization and preservation of their ways. Within Native communities, the trend is to become more in tune with their cultures as a form of healing. For years, Native ways were not practiced which permitted the prevalent historical trauma to take its toll. COVID-19 presents a real threat to the knowledge the elders hold. The elders are the keepers of the language, the traditions, the stories—their presence ensures the next generation will possess valuable knowledge to prevail.
Stacey fears people will die alone. “The resources are so limited,” she explains. “There is no hand sanitizer. Some people don’t have running water.” As soon as the local stores get supplies, they are gone. Despite being at high-risk for contracting COVID herself, Stacey checks on her elderly next-door neighbor who is 80 and, likewise, suffers from several high-risk factors that make her a prime candidate for the virus.
Not only are the elders at risk but also the youth. It is hard to put into words the dangers COVID-19 present to children, especially because, initially, the virus was presented as a threat to people over 60. However, several Native American children fall into the high-risk category. According to the OMH, “American Indian/Alaska Native children are 60% more likely to have asthma as non-Hispanic white children.” Other sources confirm that Native youth also experience higher rates of bronchitis and pneumonia than other ethnic groups. Additionally, many suffer from food insecurity which leads to malnutrition and poor health—“One out of every six children [in South Dakota] is at risk of going hungry.”
Find ways to help those in need
These are trying times for all, and many of us wonder what can be done to help. Stacey reminds all of us, “If we really, truly, just helped each other…we would be a better community. Look how creative everyone has gotten, and even though there is a pandemic going on, people are continuing to help in whatever way they can.”
.jpg?width=600&name=IMG_0920%20(1).jpg)
Native Hope encourages support of tribal organizations and community leaders. Currently, many reservations have “Stay in Place” orders, so it is vital to seek out ways to help that will not harm these communities. We are grateful for your support of our Back to Basics program as these funds have allowed us to provide much-needed food and supplies to the Lower Brule and Crow Creek reservations. We appreciate the support from tribal leaders, and community liaisons and agency directors who are reaching out and making deliveries on behalf of Native Hope.
Throughout this crisis, Native Hope continues to support those in need. We understand the spirit of giving and power of storytelling. Philámaya to our healthcare providers in all healthcare systems who are fighting for our stories to continue.
Stay home. Stay safe. Flatten the Curve.



COMMENTS